Treating dehydration in kids
Dehydration is a common reason children end up in the Emergency Room. Significantly dehydrated children often need IV hydration, but mild dehydration can often be treated at home.
For signs of dehydration by age, see this post.
Oral rehydration can be a good approach for mild symptoms but it is important to discuss with your pediatrician to determine at what point you need to step up the level of care. These are simply guidelines, but they cannot replace an individualized assessment and plan made with your doctor. If you would like this information as a free handout with step-by-step instructions, check out the guides page.
If any symptoms persist beyond 24h, it is always worth calling your doctor.
Oral rehydration: the basics
The three most important principles to oral rehydration are:
Start low
1-2 teaspoons every 5-10 minutes for babies 6 mo - 1 year
2-3 teaspoons every 5-10 minutes for toddlers 1-2 years
2 tablespoons every 5-10 minutes for children over 2 years
Go slow
Use clear liquids
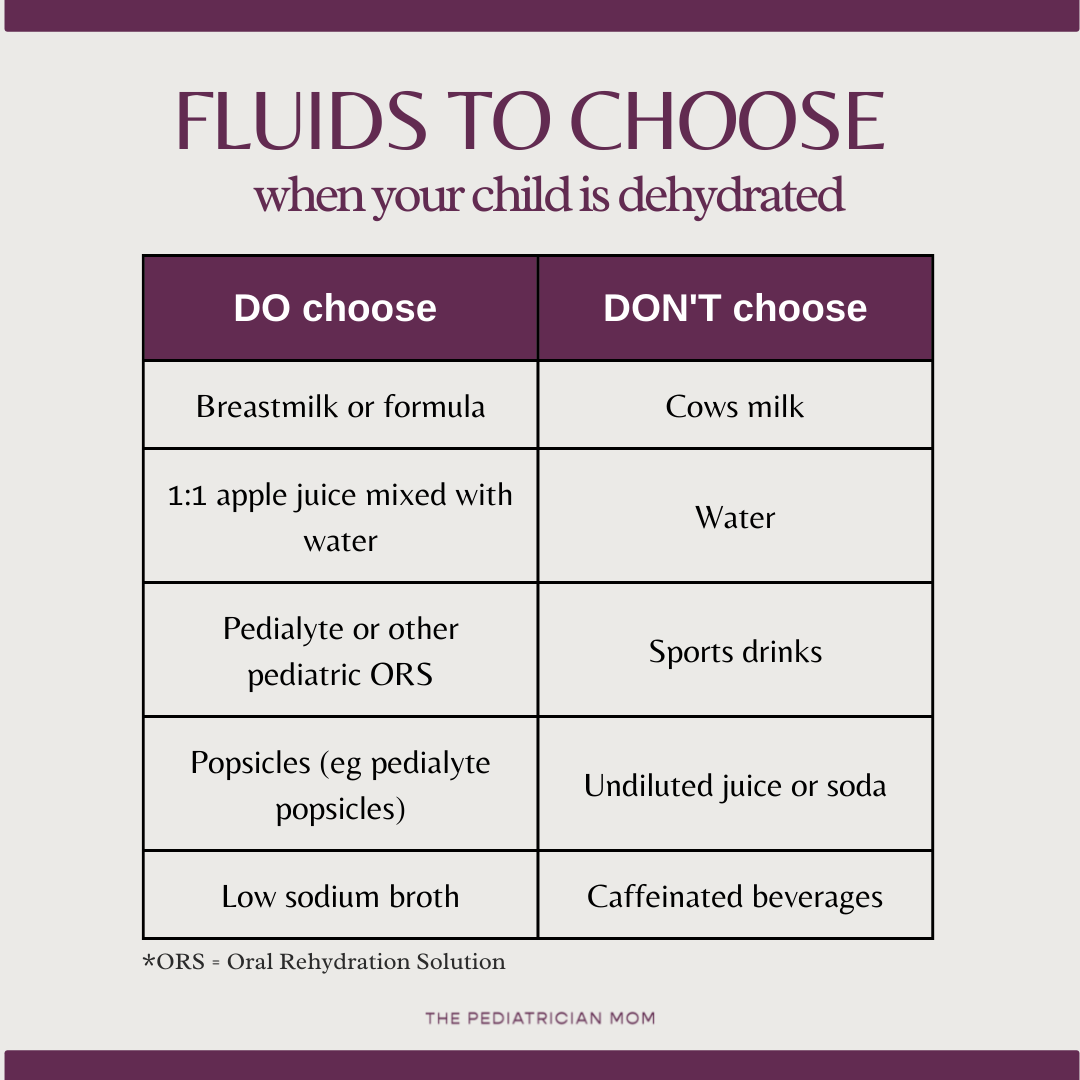
Certain fluids are better for effective rehydration. Fluids designed for this purpose are called oral rehydration solutions (ORS), but breastmilk is also a great option. For infants on formula, an oral rehydration solution is fine to start with but switch back to formula within 24h once vomiting has subsided, good option. There are also certain liquids to avoid, including water, soda, caffeinated beverages and concentrated juices.
What drinks are recommended for oral rehydration?
Frequently Asked Questions
What if my child vomits during the initial phase?
Wait 30-60min and then try again. If the vomit is recurrent or you feel they are getting more dehydrated, call your pediatrician.
My child is refusing to drink from the bottle or cup. What do I do?
You can use a syringe or a a spoon. Even young infants can actually take fluid from a spoon!
My child is hydrated and keeping things down. What are other ways to help boost fluid intake?
Try popsicles, smoothies, and foods with high water content such as cucumbers, watermelon.
What about breastfeeding or formula feeding infants?
Breastmilk is a great option for oral rehydration in infants because it is easy to digest, similar to clear liquids. For infants on formula, pedialyte can be used in the initial phase of oral rehydration, but switch back to formula within 24h. For those under 6 months, always discuss with your pediatrician first.
Why don’t you recommend concentrated juice or sports drinks?
Sometimes the high sugar content in these beverages can actually cause diarrhea and exacerbate the problem. One exception is half-strength apple juice, which has been shown in clinical trials to be as effective as oral rehydration solutions (PMID: 27131100).
What about water?
When you are sweating excessively, or losing volume due to diarrhea or vomiting, you don’t just lose liquids. You also lose electrolytes. Although plain water would replenish the fluid, it won’t replenish the electrolytes - and it can lead to severe imbalances.
What about cows milk?
Cows milk is harder to digest than clear liquids, so it is not recommended for oral rehydration. In a child with gastroenteritis, you can also see a transient lactose intolerance, so this may exacerbate their GI symptoms.
With that said: at the end of the day, your most important goal is to get your child hydrated. If cows milk is all they’ll drink, then roll with it. Just monitor closely for some worsening.
When can I offer food?
As parents, we get very worried when our children don’t eat, but during an acute illness, it is normal to lose your appetite! Focus primarily on the fluid intake. If your child is interested in solid food, and is managing to keep down fluids for 2 hours, its fine to offer foods! But once again, go slow!
There is no evidence to support use of the BRAT diet :)
How much is a goal volume for my child?
Standardly, we recommend approximately 50ml/kg of weight given over 4 hours, which is about 1ml/kg every 5 minutes. If math makes your head spin, head over to the guides page for a free download that makes it easy!