Does my child have an ear infection?
Ear infections are very common, but their symptoms can be non-specific and vague. Here is an overview of how to tell if your child has one, how we treat them, and when to call your doctor.
If you’re interested in why infections happen (and why kids are more likely to get them) and risk factors, check out this article.
Ear infections: the basics
Types of ear infections
As a reminder, there are two main types of ear infections.
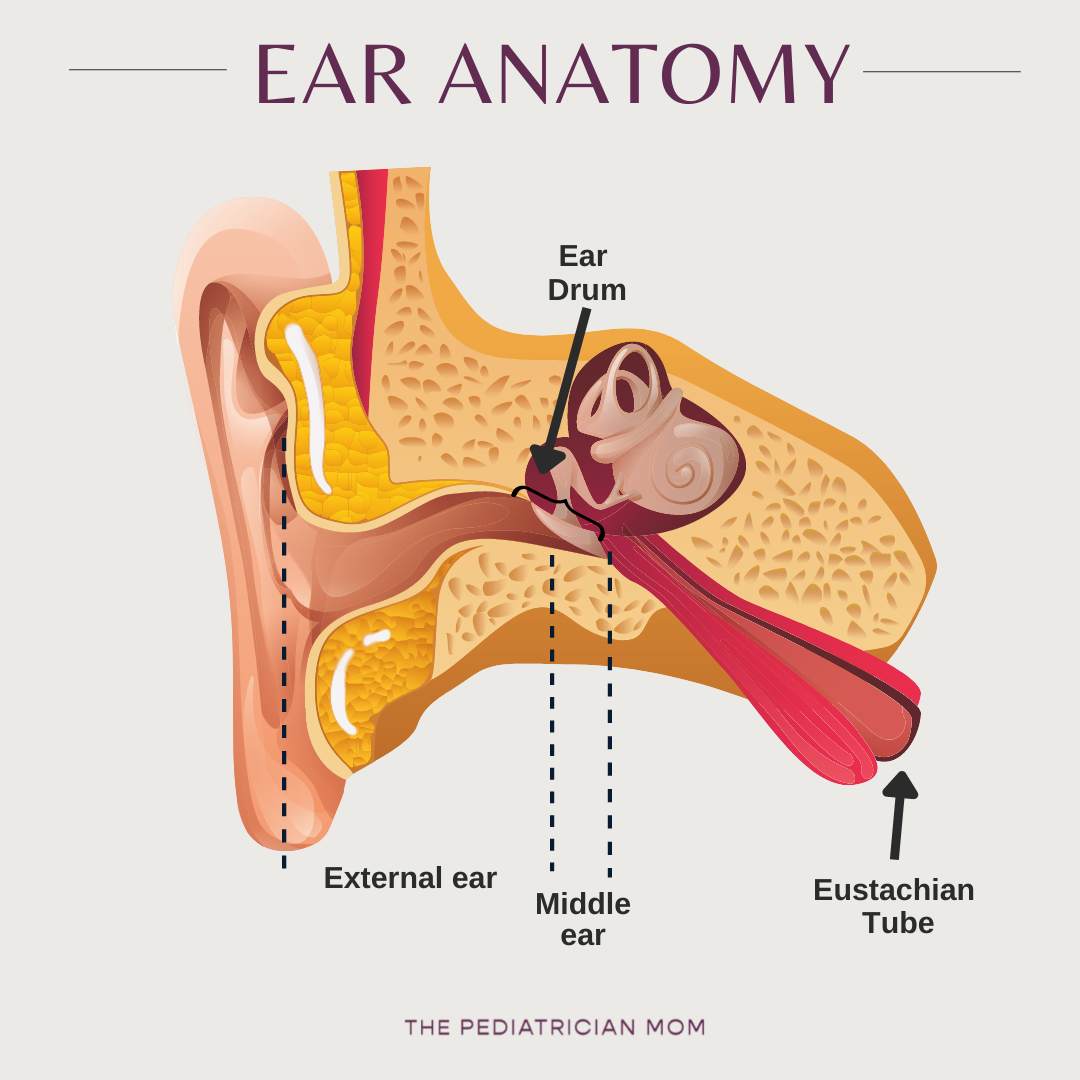
Otitis externa: an infection of the external ear. This is less common in infants and toddlers.
Otitis media: an infection of the middle ear. These are far more common in infants and toddlers and will be the focus of this post.
The two sections are separated from each other by the ear drum (or tympanic membrane).
How can I tell if my child has an ear infection?
Some common signs of ear infections include:
Fever
Pain or fussiness, especially with pressure changes in the ear (so when changing position eg when you lay your child down for a diaper change or at naptime/bedtime)
Pulling at ears or head tilting
Drainage from ears (otorrhea)
Difficulty feeding (sometimes as they try to suck the pressure changes in the ears can cause pain), or feeding less
Other indicators that are less specific, but often come up:
Sudden changes in sleep
Vomiting
Older children may complain of ear pain or difficulty hearing.
Diagnosing middle ear infections
In general, because the symptoms of ear infections are so non-specific and infants and toddlers cannot tell you their ear hurts, the only way to know definitively is to have the ear examined.
When we look inside the ear canal, we are typically looking at the ear drum to see if it is inflamed or bulging (or perforated). If it is bulging because of fluid, we pay attention to whether that fluid is clear (serous), bloody, or purulent (filled with pus).
How to hold your child for an ear exam
Many doctors have specific positions they prefer for ear examination, and they will give you instructions.
My preference allows for comfort positioning but does require a nice firm grip from the parents.
Have child sit on your lap facing you with one leg on either side, so you are chest to chest.
Hold their arms underneath your arms and wrap one hand around them in a bear hug with their head turned to one side.
The doctor can position the head and hold it steady for the exam.
The Pediatrician Mom Tip: It is counter-intuitive, but you need to hold your child firmly during an ear exam. They will squirm and scream, but if you have a wishy-washy grip, it prolongs the entire exam — and can risk injury to the ear canal.
Treatment decisions
Clinical judgment is an important factor when it comes to treatment. There are 2 possible approaches:
Antibiotics (choice is based on which bacteria are most likely to be the cause)
Watchful waiting along with managing pain (esp with kids >2 years)
With younger infants we often opt to go ahead and treat with antibiotics, and for children above 2 years, clinicians may start with observation. Being careful about antibiotic use is important not just because of increasing resistance, but also because in many cases the infection will clear without them.
For children with a history of recurrent ear infections, underlying immune issues, hearing loss or speech delay we are more likely to go ahead and treat. The AAP guidelines provide more information.
Ear tubes/tympanostomy tubes
How do ear tubes work?
Ear tubes simply create a hole in the ear drum to provide an alternate pathway for fluid to drain.
For children with recurrent ear infections, they also allows us to treat with antibiotic drops rather than oral antibiotics, because of the availability of a direct pathway to the infected fluid.
Who gets ear tubes?
Clinical judgment plays a role in deciding whether or not to proceed with surgery, but there are certain factors that make it more likely (PMID: 35138976)
Frequent ear infections: more than 3 infections in 6 months OR more than 4 infections in a year (with at least one within the preceding 6 months).
Chronic fluid: If fluid is not clearing between infections, despite treatment and time
Speech delay or hearing issues
Develops C. difficile: This is a severe post-antibiotic diarrheal infection. In these children, avoiding frequent oral antibiotic courses is important.
Other criteria: Parents, pediatricians and ENT specialists often consider other factors as well. For example, tube placement may be considered for children who are unable to take the medications, who require multiple courses of antibiotics to clear a single infection, or who are at higher risk for speech, language or learning problems such as those with underlying visual impairment, pervasive developmental disorders, or baseline hearing loss not from ear infections.
When to call the pediatrician
This is not a comprehensive list. In general, always err on the side of calling your pediatrician if you have any concerns about your child. There is a lot to be said for a parent’s gut instinct, and I promise: your pediatrician would rather you called!
If you suspect an ear infection, you should have a healthcare provider look inside the canal.
If your child is being treated for an infection and you don’t see an improvement within about 24-48 hours, or they seem worse, reach back out to your doctor.
For kids < 2 years, or those with underlying language issues, make sure you follow up for an ear recheck 2-3 months after any infection.
What can I try at home?
I just added a free download in the guides section with tips!
FAQs
Is there anything I can do to prevent them?
Check out this post for info on this.
Why do we sometimes say to watch and wait?
In some cases, an ear infection may be caused by a virus, and if this is true, antibiotics will not help (and may cause side effects and increase bacterial resistance).
The second reason is basically to do with anatomy: as I mentioned, when germs enter the eustachian tube, they cause inflammation and narrowing. This means fluid collects behind the narrow point, so when we look in the ear we see fluid. Just because the fluid is present does not mean it is necessarily infected, and over the course of the illness, that inflammation will likely improve - which means the canal should open up and the fluid should drain out.
Of course, sometimes a fluid collection itself may lead to a secondary bacterial infection. Often-times it is hard to predict which direction things will go - I often have patients come back in to look at the ear again before jumping to antibiotics, especially if the fluid looked clear rather than full of pus.
Are ear infections contagious?
No, but the associated upper respiratory infection symptoms that sometimes come with them can be contagious. Talk to your doctor if you’re unsure.
Should I put garlic, olive oil, essential oils, or anything else in my child’s ear?
Please do not do this. If there is a small perforation in the ear drum you risk exposing the middle ear to these products.
What about older kids?
Ear infections can occur at any age but they are less likely as children get older because the Eustachian tubes are no longer as small or oriented horizontally.
Older children can, of course, tell you if their ear hurts, which makes a big difference! We do tend to see more cases of otitis externa, or Swimmers ear, in older children - a topic for another day!